To be honest, I possibly had the worst immunology professor ever. She was inattentive, always late, and made us memorize the intricacies of the immune system and then regurgitate them for multiple choice exams. I was 20, I didn’t care.
No one did and no one generally does until something goes haywire with their immune system then they become acutely aware of its importance.
As students, we just wanted an A because it was a weeder class for Med School. Now that I no longer need to impress anyone with letters and numbers on my transcript, I don’t care about knowledge. I care about real understanding, subsequent action, and being able to explain complex topics simply.
You may not care for all the big words that revolve around immunology, but I hope by the end of this article you have a respect for how complicated and essential this system is to your everyday life. The system of food immunoreactivity.
In order for us to have an insightful discussion about chronic infections, autoimmunity, and food immunoreactivity, we have to have a basic understanding of how this whole thing works.
This can be tough as the immune system has all these branch thingies, lots of different cell types, and tons of fancy words like Cytotoxic Killer T Cells and Interleukin-1.
This protective and potentially destructive system is stupid, but at the same time, incredibly intelligent. Recently there has been a lot of yelling on the internet about the immune system as it relates to food and I feel that many people are quite confused about this subject.
Thus, I want you to be able to discern what part of that conversation is just noise and what part is legitimate.
The Two Types of Immunity
The Innate Immune System or Non-Specific Immune System
This branch provides immediate defense against an infection. The innate immune system includes cell like Natural Killer Cells, Mast Cells, Macrophages, and Dendritic Cells.
The Adaptive or Specific Immune System
This branch is much more sophisticated and highly specific. This system itself also has two branches cell mediated and humoral immunity. The adaptive immune system is made up of B and T lymphocytes.
Sooo many words…let’s watch a Moooooovie or two.
Immune System Overview
Adaptive Immunity Overview
Immunoreactivity to Common Foods
Now that we have some understanding of Immunology under our belts, we can get to the meat of what my clients tend to care about – immunoreactivities to common foods and how this can be a trigger for autoimmunity or one’s own immune system seeing self-tissue as a pathogen.
This is a very big deal as it is estimated that over 50 million Americans suffer from some kind autoimmunity (comparatively, heart disease “only” affects upwards of 22 million Americans) and the occurrence of autoimmunity is growing exponentially.
It is now believed that around 30% of autoimmunity is due to genetic predisposition. But, this means that 70% of autoimmune cases are potentially caused by environmental and lifestyle triggers – the main culprits being intestinal permeability, infections, and chemical exposures.
“Bacterial toxins, chemicals, foods, and undigested proteins and peptides can induce systemic food immune reactivity by causing failure of immune tolerance. Immune tolerance is the immune system’s ability to recognize what is harmful and what is not. If immune tolerance is lost, then inflammation ensues and autoimmunity can occur.”
– Andrew Campbell MD
The digestive system sees over 1 ton of food each year and contains north of 70% of our immune cells. Your GI tract also has more contact with the outside world than your skin and this mucosal lining is constantly being exposed to potential antigens.
The reason our body does not wreck shop on all this food stuff all the time is because of oral tolerance which occurs through the deletion or immunosuppression of reactive immune cells.
Reacting to common food items is not normal and may be due to impaired immunological development (which is outside the scope of this post and revolves around the hygiene hypothesis, maternal diet, how one was born, breast feeding, and the infant gut microbiota) or an immune system that is out of balance (cough low vitamin D) and over stimulated (SAD).
Thus, if you were a bottle-fed C-section baby who took anti-biotics all throughout childhood, you are going to be at much more at risk for losing oral tolerance. I have seen these patients’ food panels and they light up like a Christmas Tree. It sucks.
Also, if you are frazzled, consuming copious amounts of alcohol and caffeine, never outside, drinking scandalous water, don’t sleep, and are crashing face first into the Standard American Diet (SAD) of inflammatory processed foods that the human body has never seen before, you are going to be pushing your luck as well.
Enter intestinal permeability – which as Dr. Rakowski says, “In our current environment we are all leaky, it is just a matter of how much.” Intestinal permeability or leaky gut is induced by dysbiosis, gut pathogens, NSAIDS, chronic exercise, traumatic brain injury, stress, and basically any other inflammatory reaction in the GI tract.
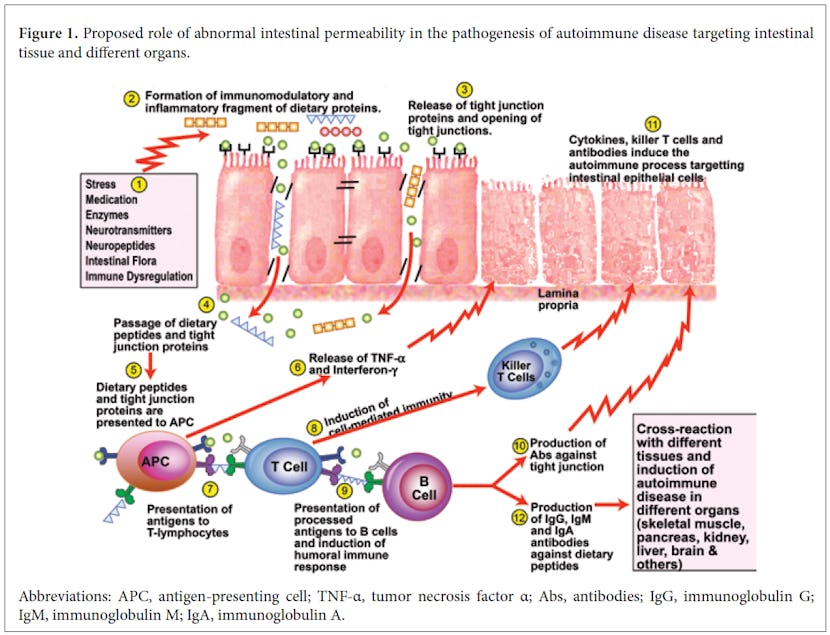
The figure above is from Dr. Aristo Vojdani, one of the leaders, if not the leader, in food immunoreactivity. There is a lot going on above, but we can use our newfound understanding of immunology and begin to grasp how this all works.
What Happens in Your Digestive Tract
An Antigen Presenting Cell (APC) (these cells are constantly sampling everything in the digestive tract) encounters a peptide which is bigger than it ought to be. Maybe this is gliadin (a component of gluten) which our body doesn’t have the machinery to digest very well, it then presents this antigen to the T-Helper Cell which can induce cell-mediated immunity (a Th-1 response) which will create a fight in the guts and thus, inflammation, and more leakiness.
T-Helper Cells can also induce humoral-mediated immunity (a Th-2 response) which will result in the activation and proliferation of B cells into plasma cells which will produce antibodies against this specific protein (this is what we are investigating with Cyrex immunoreactivity testing).
Our immune system has tagged this peptide for destruction and will now also remember this protein/antigen and react to it faster and more aggressively the next time it comes down the chute.
The hook is that what happens in the gut, doesn’t stay in the gut and these food particles can look a lot like our own tissues.
For example, gluten looks a lot like the tissue of the cerebellum and can result in the immune system seeing that part of your brain as foreign and then you can be left literally stumbling around with something called cerebellar ataxia all because you really like bagels.
Gluten is also implicated in many cases of Hashimoto’s – which is autoimmunity to the thyroid gland. Hashimoto’s is the most prevalent autoimmune condition with an estimated 20 million Americans having some form of thyroid disease and 80-90% of those being Hashimoto’s cases.
Whew, that is definitely enough for one day; but if this piqued your interest, I would implore you to watch more videos and read more on this subject as it is a relatively new frontier and we as a scientific community, by no means, have this all figured out yet.
But, now that we have the foundation laid, when people start chattering about how they can’t eat this or that, you can choose to speak or not, but at least you will be able to identify when someone is just spewing nonsense in-between bites of spaghetti.
If you just can’t wait for more information on this topic, Chris Kresser has a fantastic and detailed discussion here.
“Today’s clinician is faced with patients whose initial symptoms are vague and nonspecific, such as fatigue, joint aches and pains, sleep disturbance, brain fogginess, wide mood swings, cognitive function problems, changes in bowel habits, numbness and tingling, and a general feeling of malaise. There is good news in all this: There are laboratory analyses that can detect these antibodies early, years before the reactions with the immune system appear that cause the irreversible and chronic damages that lead to autoimmunity.”
– Dr. Andrew Campbell
More picking on gluten… If I get sued by Cinnabun™ for using this image, then so be it.
“I write posts hoping 20,000 people will love them, not that 1,000,000 people will like them.”
-Tim Ferris
This article is that type of post. Some people don’t want to know the nitty gritty; they just want to drink the Kool-Aid™. That’s fine, but every one of my clients, friends, and colleagues (some of these folks have taught me this stuff) deserves to know the why.
Earlier, we spoke about how larger proteins can activate both cell mediated and humoral immunity within the submucosa of the GI tract. AKA, when bigger stuff that is not supposed to pass between tight junctions slips through, and then the immune system reacts to said bigger stuff (proteins larger than 5,000 daltons), even though it’s not supposed to.
In the words of Dr. Rakowski, “How does a hurricane happen? When the conditions are just right.”
What are the conditions that bring on the storm of food immunoreactivities and autoimmunity? Intestinal permeability, a dysregulated and over stimulated immune system, environmental toxins, latent infections, and a diet chock full of processed garbage.
What to Do If You Have Food Immunoreactivity
So what can we do about all this?
Well, it’s fairly simple.
Heal the digestive tract, regulate the immune system, limit environmental toxins, identify and treat any underlying infections, and replace processed garbage with real food that we can digest, assimilate, and eliminate without immune burden.
BUT, what if we are already in the storm???
Fundamentals! We do the same thing, but now we have to cut out any foods or environmental triggers that are immune stimulatory.
This means that we need to run further testing, as now someone could be immunoreactive to anything that they eat like coffee, chocolate, tomatoes, spinach, kale, or even non-gluten grains. Cyrex Labs is the gold standard for food immunoreactivity.
They are expensive, but I have tried other labs, and no one comes close to the ship that they drive. They run all their arrays in duplicates to double check themselves and have the purest and most specific antigens.
What Cyrex is testing for in arrays 3, 4, and 10 are Immuoglobulin A (IgA) and Immunoglobulin G (IgG) antibodies to different food proteins.
Now we get into the intricacies of humoral immunity. Yes!
To review from earlier in the article, we will use a figure from a fantastic lecture by Dr. Fasano. Everyone should watch it. Not only is he a great scientist and leader in the field of celiac disease, but he is also a very entertaining speaker.
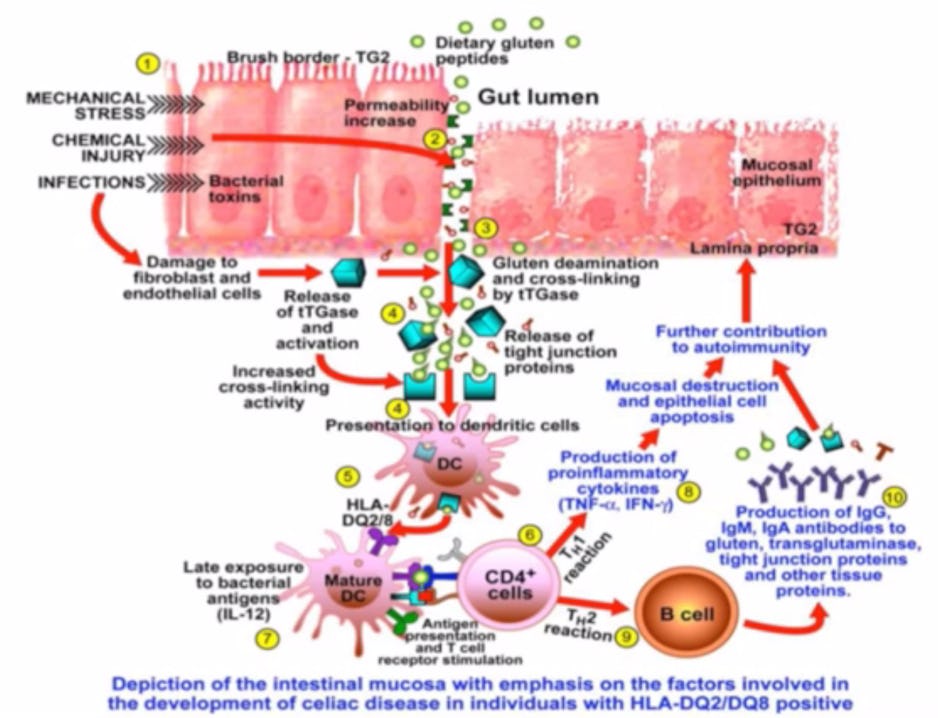
A bigger than it should be dietary peptide gets through tight junctions. An APC then presents this antigen to the T-Helper Cell (CD4+), which can activate Cytotoxic Killer T Cells (CD 8+) to starts wrecking shop and can also present the antigen to B Cells that then differentiate into plasma cells and start spewing out antibodies or immunoglobulins systemically, specifically IgA, IgG, and IgM.
You may now be like… what about IgE? IgE reactions are food allergies. These invoke very quick responses, think anaphylaxis and epi pens from a peanut allergy.
If you get a post nasal drip after consuming dairy, this is likely a food allergy producing a fast IgE response, not a food immunoreactivity. This is also what they test when you go to the allergist and they prick you with all sorts of antigens.
What we are talking about above is different. Food immunoreactivities are generally more insidious and lead to what I call feeling like shit-itis. Some clients feel amazing after removing the culprits, but others need much more than avoiding specific immunoreactive foods to get things back online.
Regardless, we will never gain any ground without this step. And for those with autoimmunities, regulating the immune system and calming the storm will be their life’s work because as of now, we do not have a means to get the immune system to unsee one’s own tissue as a foreign pathogen.
I do think someday we might, but until then, we as clinicians have to help patients improve vitamin D and glutathione status, heal the GI tract, avoid environmental triggers and reactive foods, and quell inflammation with appropriate supplementation.
Dang… you guys killed it, and now you can can choose whether to help your annoying uncle who is gluten free but still pounds eggs, diary, soy, and rice or not.
This information, if delivered correctly, may help him realize he is not an expert and that he is just following the sheep to the frozen bread aisle.
This process is bigger than gluten. Gluten is just a highly reactive big protein we like to pick on. This is about personalization and that means finding out what works for you through elimination and reintroduction protocols and also objective testing when necessary.
If you would like to start this process, we don’t typically begin with Cyrex testing, as there are some fundamental steps we have to go through before ordering five hundred to a thousand dollars in food immunoreactivity panels.
However, if you have an autoimmune disease, I would start this process right now right now.

)